Dr. J and Dr. I visited the Fox 32 Chicago News at Noon with Sylvia Perez during Allergy and Asthma Awareness Month to both discuss some surprising causes of asthma and allergies and some surprising ways to control them.
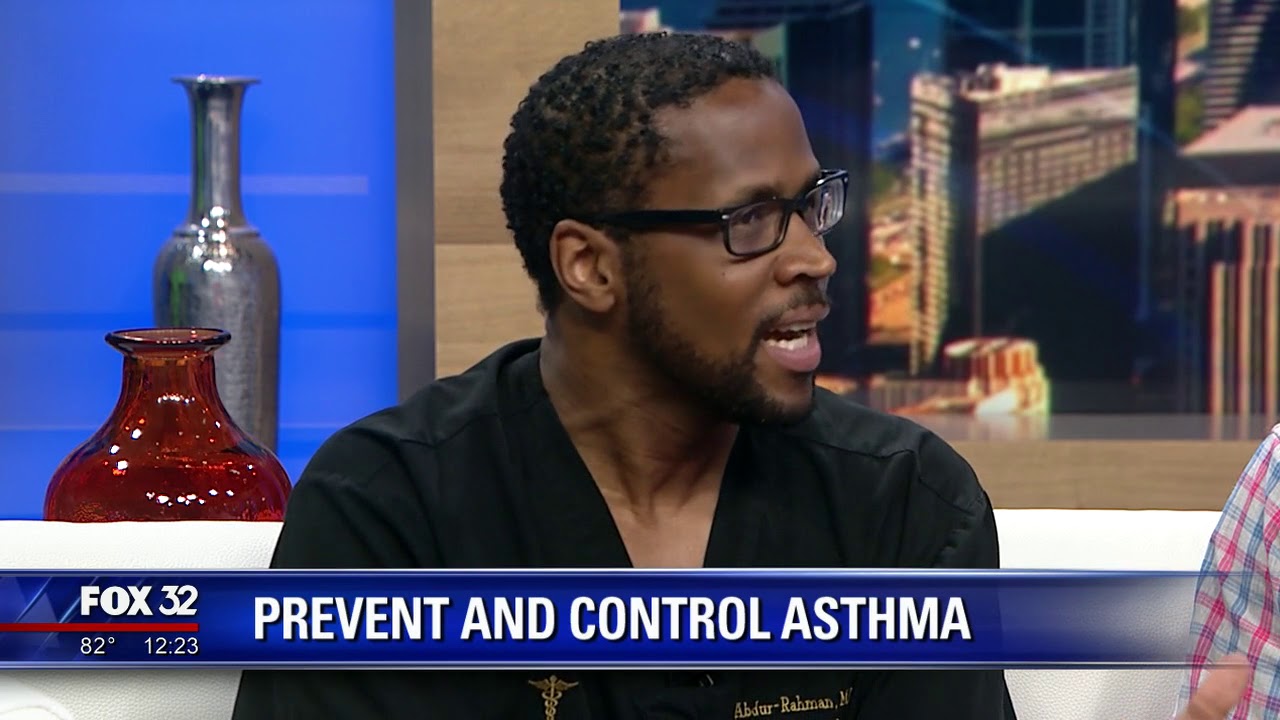
Dr. J and Dr. I visited the Fox 32 Chicago News at Noon with Sylvia Perez during Allergy and Asthma Awareness Month to both discuss some surprising causes of asthma and allergies and some surprising ways to control them.


TheTwinDoctors.com is the creation of twin OB/Gyn Doctors Jamil and Idries Abdur-Rahman. Jamil (Dr. J) and Idries (Dr. I) were inspired to start TheTwinDoctors.com after participating on season 22 of CBS’ ‘The Amazing Race’.
by Idries Abdur-Rahman (Goodreads Author),
Jamil Abdur-Rahman MD, Nikia Bilal (Editor)
 October 4, 2018
October 4, 2018
The Mucus Plug, Can You Lose It Twice?
 November 14, 2017
November 14, 2017
Pre-Ejaculate, Can You Get Pregnant From It?
 November 11, 2017
November 11, 2017
Postpartum Vaginal Pain And The Witch Hazel Fix
 November 9, 2017
November 9, 2017

From Baby Bumps to Burp Me Your Guide to Pregnancy and Parenthood

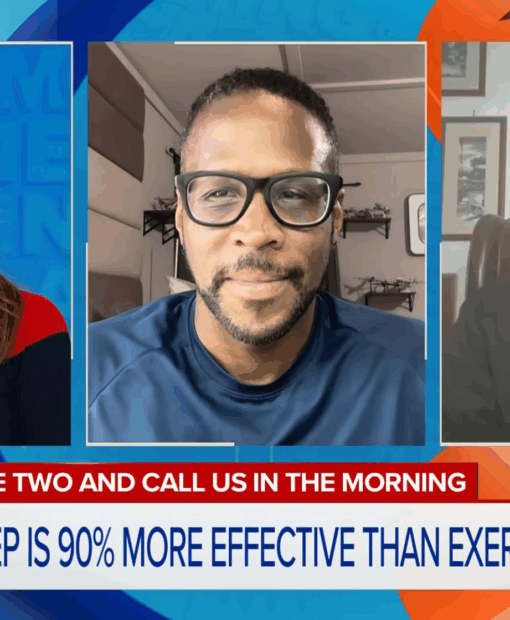
Exercise vs Sleep, Only One Can Win!

© 2026 TheTwinDoctors.com. Copyright 2020-2025 TheTwinDoctors.com. All rights reserved.