5 things that can go wrong with your IUD and what to do about it.
 May 19, 2018
May 19, 2018
What Is Chlamydia
Chlamydia is an extremely common sexually transmitted disease that is caused by the bacterium Chlamydia Trachomatis. The U.S. Centers For Disease Control estimates that close to 2,000,000 Americans have Chlamydia. While both men and women can become infected with Chlamydia, women are three times more likely than men to have the infection. People under the age of 30 are also the most likely to be infected with Chlamydia than are people over the age of 30.
Chlamydia Frequency By Age
The vast majority of people with Chlamydia get the infection after they have had unprotected sex with someone who is infected by the bacteria. In rare cases however, Chlamydia infections of the eyes can be seen in newborn babies that are born to mothers with active Chlamydia infections at the time of delivery. When Chlamydia is transmitted through sexual activity however, it can be transmitted by vaginal, oral and anal sex.

What are Symptoms of Chlamydia
One reason that Chlamydia is so prevalent is that many people with the infection have no symptoms of the infection. In fact, 50% of women with Chlamydia and 75% of men with Chlamydia have no symptoms of the disease. As a result, a majority of people infected with Chlamydia may be unaware that they have the disease. Unaware, they may then unknowingly pass it from one unsuspecting partner to another. When symptoms of Chlamydia are present however, they include;
Chlamydia is most frequently diagnosed using NAA (Nucleic Acid Amplification) tests. NAA tests are the preferred method for diagnosing Chlamydia because they test for the actual presence of the bacteria’s DNA in a person’s body. Typically, if DNA from the Chlamydia bacteria is found in a person’s body, then they have Chlamydia. NAA tests therefore are very accurate. NAA tests for Chlamydia require either collecting a person’s urine or swabbing their vagina (in the case of women) or their urethra (in the case of men).

Urine Testing for Chlamydia
When urine is collected to test for the presence of Chlamydia, it should be a “first catch” sample. This means that the urine sent to the lab for testing should be the urine passed as soon as a person starts his or her urinary stream. Ideally the first 20ml of urine voided should be collected. The initial urine voided is the urine that is most likely to contain DNA from the Chlamydia bacteria. The urine that is passed as the urinary stream is ending on the other hand tends to be more diluted, making it less likely to contain large amounts of Chlamydia DNA. Once collected, urine is sent to the lab where it is tested for the presence of Chlamydia DNA. Typically, results will come back within 2-3 days of the urine having been collected.

Chlamydia Swab Testing
Swab NAA testing involves a cotton swab being placed in the vagina or the urethra. Secretions found in the vaginas and in the urethras of people with chlamydia infections will frequently contain large amounts of bacteria’s DNA. This DNA will therefore be captured by the testing swab. When the testing swab is sent to the lab, it can then be analyzed for the presence of chlamydia DNA. Typically, it takes 2-3 days for results to come back.
If Chlamydia is not treated, a number of potentially serious health complications can result. These complications can include pelvic inflammatory disease (PID), ectopic pregnancy, infertility and blindness.
Pelvic inflammatory disease results when a woman’s pelvic organs including her cervix, uterus, Fallopian tubes and ovaries become infected. The infected pelvic organs then become swollen and inflamed, which is why “Pelvic Inflammatory Disease” is called pelvic inflammatory disease. Most commonly, pelvic inflammatory disease is caused when the cervix, uterus, Fallopian tubes and ovaries are infected by sexually transmitted diseases like Chlamydia and Gonorrhea. Pelvic inflammatory disease does however sometimes result from infections caused by non-sexually transmitted diseases. Early on, women with pelvic inflammatory disease may not have any symptoms. However, as pelvic inflammatory disease progresses, women may have the following symptoms:
Untreated, pelvic inflammatory disease can quickly progress, leading to a potentially life-threatening pelvic abscess. Pelvic abscess that resulted from untreated pelvic inflammatory disease typically develop in the Fallopian tubes and they are called Tubo-Ovarian Abscess (i.e. TOA). Patients with TOA’s are often very sick; frequently requiring hospitalization, the administration of very potent IV antibiotics and sometimes even surgical intervention to remove the pelvic abscess.
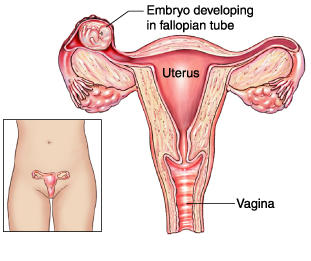
Ectopic Pregnancy
An ectopic pregnancy refers to a pregnancy that is growing somewhere other than inside of the uterus (womb). 98% of ectopic pregnancies occur in the Fallopian tubes. This is because all eggs when fertilized by sperm are actually fertilized in the Fallopian tubes. Once fertilized in the Fallopian tubes, the fertilized eggs then normally move from the Fallopian tubes to the uterus where they implant and begin to grow. In the case of ectopic pregnancies however, once fertilization of an egg has occurred in the Fallopian tube, the fertilized egg gets trapped in the Fallopian tube.
Fertilized eggs are more likely to get trapped in the Fallopian tubes after someone has had a chlamydia infection because chlamydia frequently causes inflammation of the Fallopian tubes. Inflammation of the Fallopian tubes can then causes scarring of the Fallopian tubes, and scarred Fallopian tubes no longer function properly. Malfunctioning Fallopian tubes often trap fertilized eggs.
Unlike the uterus which is fairly large, Fallopian tubes are too small to accommodate a growing pregnancy. This means that as an ectopic pregnancy grows in the Fallopian tubes, it causes them to stretch. If untreated, a growing ectopic pregnancy will eventually become too large for the Fallopian tube, causing it to stretch and then rupture. A ruptured Fallopian tube can become a life-threatening emergency as it can lead to massive bleeding in the belly.
Chlamydia infections frequently cause inflammation and swelling of the uterus and the Fallopian tubes. Inflammation of the uterus and the Fallopian tubes, if severe enough, can cause scarring of the uterus and Fallopian tubes. Because fertilization of eggs by sperm occurs in the Fallopian tubes, and because fertilized eggs then migrate from the Fallopian tubes to the uterus where they grow and ultimately lead to a pregnancy; when the uterus and the Fallopian tubes have become scarred and damaged by a chlamydia infection, it can become very difficult for a woman to become pregnant. In fact, 12% of women who are diagnosed with pelvic inflammatory disease after suffering a chlamydia infection will later suffer from infertility.

Adult Chlamydia Eye Infection
Chlamydia can infect the eyes. In adults, this is rare. When seen in adults however, chlamydia infections of the eyes most frequently result from a person with the bacteria on their hands rubbing their eyes. It also can result when a person washes their face with a wash towel that someone with chlamydia has used to clean their private parts.

Newborn chlamydia eye infection
Chlamydia infections of the eye are most frequently seen in newborns. When a newborn baby passes through the birth canal of a mother who has an active chlamydia infection, their eyes may be exposed to the bacteria causing a chlamydia eye infection. A chlamydia infection of the eyes can then cause scarring of the inner eyelids. Scarred inner eyelids can then become rough and abrasive. Rough and abrasive inner eyelids can then irritate the cornea of the eye. Prolonged irritation of the cornea can ultimately lead to its breakdown and then to blindness.
Chlamydia is treated by using antibiotics. For most uncomplicated cases of chlamydia, oral antibiotics like Azithromycin, Doxycycline and Erythromycin will eliminate the disease. Sometimes, more complicated cases of chlamydia like those that involve the development of pelvic inflammatory disease or a tubo-ovarian abscess (TOA) may require hospitalization and the administration of IV antibiotics like doxycycline, levofloxacin or ofloxacin. Once chlamydia has been treated, testing for the bacteria should be repeated within 3 months of the treatment. This is done to help ensure that the infection has completely resolved. Additionally, when a person is treated for chlamydia, their sexual partner(s) should also be treated. And all parties should then wait at least 2 weeks after treatment before resuming sexual activity.