5 things that can go wrong with your IUD and what to do about it.
 May 19, 2018
May 19, 2018

Thyroid Gland
Every cell in the human body uses energy to function. Much of the energy used by the body’s cells comes from the food we eat. The thyroid gland is a butterfly-shaped organ located at the base of the neck that releases hormones commonly referred to as “thyroid hormones”. These thyroid hormones are also known as “T3” and “T4”. Thyroid hormones control metabolism, or how effective the body’s cells are at using the energy released from food to power themselves when they carry out their functions. People with “high metabolism” are able to use more of the energy released from the food that they’ve eaten to power their organs. People with “low metabolism” are able to use less of the energy released from the food that they’ve eaten to power their organs.
Thyroid Disease refers to a group of conditions that can affect the thyroid gland. These conditions will either result in the thyroid gland producing too much T3 and T4 or too T3 and T4. Because thyroid hormones control how much of the body’s available energy cells can actually use to power themselves; the production of too much or too little thyroid hormone(s) can profoundly affect how well the body’s cells and organs function. If too much energy is made available to the body’s cells, they my function too much, becoming over active. If too little energy is made available to the body’s cells, they may function too little, becoming underactive. The most commonly diagnosed thyroid diseases include hypothyroidism, hyperthyroidism, Grave’s Disease, Hashimoto’s Disease and Thyroiditis.

Hypothyroidism starves the body’s cells of fuel.
Hypothyroidism results when the thyroid gland is not making enough of the T3 and T4 thyroid hormone(s). Because the body’s cells rely on thyroid hormone(s) to help them to utilize energy, when too little thyroid hormone(s) have been produced, the body’s cells run low on energy. Much like a car would struggle to function optimally if it did not have enough gas available to it, the body’s cells struggle to function optimally when they do not have enough energy available to them.
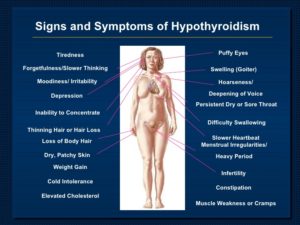
Possible Symptoms of Hypothyroidism
Every cell in the body relies on the T3 and T4 thyroid hormone(s) to function properly. Thyroid hormone(s) help the body’s cells to utilize the energy that they need to carry out their functions. When levels of thyroid hormone(s) are low, the body’s cells are not able to optimally utilize energy. Without being able to optimally utilize energy, the body’s cells run low on energy and then are not able to function optimally. Sub-optimally functioning cells and organs can of course mean different things for different parts of the body.
Hypothyroidism can cause a sub-optimally functioning “slow” brain.
If brain cells are not able to optimally utilize energy for example, the brain is not able to function optimally. This can result in brain related issues like depression and memory loss occurring. If on the other hand cells in the intestines are not able to optimally utilize energy, then the intestines are not able to function optimally. This can result in GI related issues like constipation. Because all cells in the body rely on thyroid hormone(s) to help them to utilize energy, hypothyroidism can lead to dysfunction of all of the body’s cells and organs. This is what makes hypothyroidism potentially quite dangerous.
Hyperthyroidism results when the thyroid gland is making too much of the T3 and T4 thyroid hormones. Because the body’s cells rely on these thyroid hormones to help them to utilize energy, when too much thyroid hormone(s) has been produced, the body’s cells can become “overloaded” with energy. Once overloaded with energy, the body’s cells and organs may function too aggressively, becoming dangerously overly active.
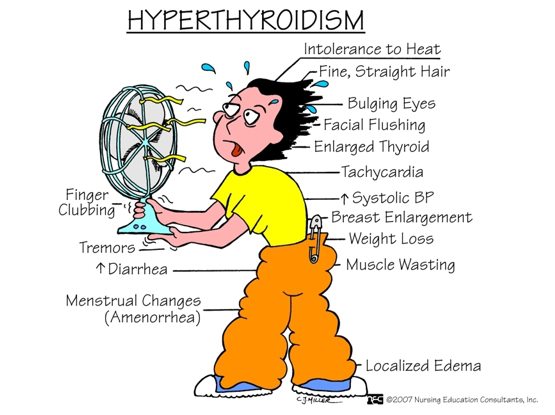
When the thyroid gland is making too much thyroid hormone(s), the body’s cells and organs become overloaded with energy. Overloaded with energy, the body’s cells and organs then “speed up”, functioning at a higher pace. This higher pace can for example cause the heart to “speed up”, leading potentially to an irregular heart beat or even to a heart attack. This higher pace can also cause the activity of the brain cells (neurons) to “speed up”, leading potentially to anxiety, mood disturbances and even seizures. Because all cells and all organs in the body rely upon the T3 and T4 thyroid hormone(s) to help them to utilize energy, an overactive thyroid gland can result in every one of the body’s cells and organs functioning at a higher than normal pace. This higher than normal pace can compromise everyone of the body’s vital functions. This is what makes hyperthyroidism potentially quite dangerous.
Grave’s Disease results when a person’s immune system mistakenly makes a protein that functions like Thyroid Stimulating Hormone (TSH). Normally, the thyroid gland releases the thyroid hormones T3 and T4 when the pituitary gland in the brain secretes TSH. The job of TSH is basically to tell the thyroid gland that it is time for it to make and release more T3 and T4 so that the body’s cells and organs can utilize the energy that they need to function properly. In Grave’s Disease however, the immune system makes a protein that the thyroid gland thinks is TSH. This confusion causes a form of hyperthyroidism as the thyroid gland starts making too much T3 and T4.

Exophthalmos (bulging eyes) seen in Graves Disease.
Common Symptoms of Grave’s Disease include the common symptoms of hyperthyroidism listed above along with two additional symptoms that are unique to Grave’s Disease. These unique symptoms include:
Grave’s Disease is dangerous because it is a form of hyperthyroidism. The potential dangers of hyperthyroidism have been listed above in the “Why Is Hyperthyroidism Dangerous” section.
The primary job of the immune system is to protect the body against both foreign invaders (i.e. viruses, bacteria, fungi, etc.) and unhealthy cells like precancerous and cancerous cells. When an autoimmune condition occurs however, the immune system becomes “confused”. In this confusion, the immune system believes that parts of its own body are foreign invaders. This results in the immune system attacking the part(s) of the body that it thinks is a foreign invader. Hashimoto’s Disease is an autoimmune disease that results when the immune system attacks the thyroid gland. This attack on the thyroid gland eventually destroys it, leaving it largely non-functional. When the thyroid gland has been destroyed it no longer produces the T3 and T4 thyroid hormones. This effectively means that someone with Hashimoto’s Disease has a form of hypothyroidism.

Goiter
Common symptoms of Hashimoto’s Disease include the common symptoms of hypothyroidism listed above. Additionally, Hashimoto’s Disease can present with the formation of a goiter. A goiter is an enlarged, inflamed thyroid gland.
Hashimoto’s Disease is dangerous because it is a form of hypothyroidism. The potential dangers of hypothyroidism have been listed in the “Why Is Hypothyroidism Dangerous” section above.
Thyroiditis results from an inflammation of the thyroid gland. Thyroiditis typically occurs in phases with the first phase of the disease being called the “thyrotoxic phase”. During this initial “thyrotoxic phase” of thyroiditis, the thyroid gland produces too much of the T3 and T4 thyroid hormones. This in effect causes someone with thyroiditis to initially have hyperthyroidism. This hyperthyroid thyrotoxic phase of thyroiditis typically lasts anywhere from a few weeks to a few months. Eventually, the initial inflammation of the thyroid gland then causes the gland to release all of it’s thyroid hormones. Once all of the thyroid hormones have been exhausted, the thyroid gland has no more T3 and T4 to release. Burned out, the thyroid gland then enters the second phase of thyroiditis. This phase is called the “hypothyroid phase” because the thyroid gland has no more thyroid hormone(s) to release. During the hypothyroid phase of thyroiditis, a patient effectively has hypothyroidism.
Depending upon the cause of thyroiditis, the hypothyroid phase of the disease may or may not be permanent. If the hypothyroid phase of thyroiditis is not permanent however, then a third phase of thyroiditis called the “euthyroid phase” occurs. During the euthyroid phase of thyroiditis, the thyroid gland recovers from the damage caused by the inflammation. With recovery, the previously burned out thyroid gland recovers it’s normal function.
The common symptoms of thyroiditis initially include the common symptoms of hyperthyroidism. As the disease progresses, the common symptoms of thyroiditis later include the common symptoms of hypothyroidism. See the common symptoms of both hyperthyroidism and hypothyroidism listed above.
Thyroiditis is dangerous because the disease is characterized by periods of hyperthyroidism and hypothyroidism. The potential dangers of both hyperthyroidism and hypothyroidism have been listed above in the “Why Is Hyperthyroidism Dangerous” and in the “Why Is Hypothyroidism Dangerous” sections.
There are a number of different ways to diagnose thyroid disease. They include:
 Feeling the Thyroid Gland: Frequently, the first steps taken in diagnosing thyroid disease will involve a Doctor “palpating” or feeling a patient’s thyroid gland. Many times when thyroid disease is present, the thyroid gland will feel larger than normal, smaller than normal, it will have multiple masses called nodules that can be felt across the skin or it will be excessively tender when touched.
Feeling the Thyroid Gland: Frequently, the first steps taken in diagnosing thyroid disease will involve a Doctor “palpating” or feeling a patient’s thyroid gland. Many times when thyroid disease is present, the thyroid gland will feel larger than normal, smaller than normal, it will have multiple masses called nodules that can be felt across the skin or it will be excessively tender when touched.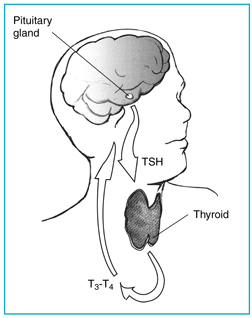
TSH for the pituitary gland in the brain tells the thyroid gland to make more T3 and T4.
gland to make thyroid hormone(s). If the thyroid gland is making too much thyroid hormone (i.e. in Hyperthyroidism, Grave’s Disease, the first stage of Thyroiditis, etc.), then the TSH level will be abnormally low. This is because there is already too much of the T3 and T4 thyroid hormones in the circulation and the pituitary gland does not want to signal the thyroid gland to produce and release anymore. If on the other hand the thyroid gland is making too little thyroid hormone (i.e. Hypothyroidism, Hashimoto’s Thyroiditis, the second stage of Thyroiditis, etc.), then the TSH level will be abnormally high. This is because there is not enough of the T3 and T4 thyroid hormones in the circulation and the pituitary gland wants to signal the thyroid gland to produce and release more.
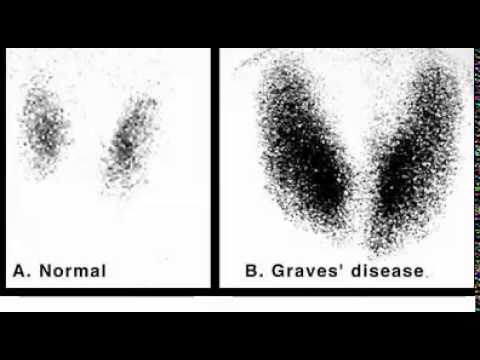
Normal thyroid nuclear scan (left) and abnormal (hyperthyroid) thyroid nuclear scan (right).
Over-active thyroids (i.e. Hyperthyroidism, Grave’s Disease, the first phase of Hashimoto’s Thyroiditis, etc.) are making too much T3 and T4. They therefore will absorb more than normal amounts of the Iodine needed to make T3 and T4. Conversely, when the thyroid is under-active (i.e. Hypothyroidism, the second stage of Hashimoto’s Disease, etc.) it is making too little T3 and T4. The thyroid will therefore absorb less than normal amounts of the Iodine that it needs to make T3 and T4. RAI-U thyroid scans can also be used to evaluate the size of the thyroid gland. In many thyroid diseases, the thyroid gland is either larger than normal or smaller then normal.

Fine Needle Thyroid Biopsy
Thyroid disease is typically treated using either a variety of different medications or surgery. The treatment approach(es) taken ultimately depend upon the thyroid disease(s) present.
Because hypothyroidism results when the thyroid gland is not producing enough thyroid hormone(s), the primary treatment of hypothyroidism involves taking synthetic forms of the T4 thyroid hormone. The most commonly prescribed synthetic forms of the T4 hormone include Synthroid and Levothroid. Once prescribed, the doses of Synthroid and Levothroid will likely be adjusted until the amount of T4 hormone in the blood is sufficient.
Hyperthyroidism can be treated using medications and surgery. The treatment approach taken ultimately can depend upon a number of different factors.

Thyroid Surgery
Grave’s Disease is a form of hyperthyroidism. Therefore, the treatment approaches to Grave’s Disease include many of the same treatment approaches taken to treat hyperthyroidism (see “How Is Hyperthyroidism Treated” above). This means that radioactive Iodine, anti-thyroid medications and thyroidectomy can all be used to treat Grave’s Disease. Grave’s Disease is sometimes associated with a finding that is unique to it, that of bulging eyes or “exophthalmos”. Unique approaches taken to treat exophthalmos include the following:
Hashimoto’s Disease occurs in multiple stages. The first stage of Hashimoto’s Disease is characterized by hyperthyroidism. The second stage of Hashimoto’s Disease is characterized by hypothyroidism. And then in some cases there is a third stage of Hashimoto’s Disease that is called the “Euthyroid” stage. During the Euthyroid stage (if it occurs), the thyroid glands returns to normal function. If the Euthyroid stage does not occur, then the second hypothyroid stage and hypothyroidism persist. Because Hashimoto’s Disease has multiple stages, the treatment of Hashimoto’s undertaken depends upon the stage of the disease.
When Hashimoto’s is in the first “hyperthyroid” phase, Hashimoto’s Disease is treated like hyperthyroidism (see “How Is Hyperthyroidism Treated” above). This can include the use of radioactive Iodine and anti-thyroid medications. When Hashimoto’s is in the second “hypothyroid” phase, the disease is treated like hypothyroidism (see “How Is Hypothyroidism Treated” above). This can include the use of synthetic forms of the T4 hormone like Synthroid and Levothroid. If the third and final “euthyroid” stage of Hashimoto’s Disease occurs, then normal thyroid function has returned and no further medical or surgical management is required.
Much like Hashimoto’s Disease, thyroiditis occurs in stages. There is an initial “hyperthyroid” stage during which the thyroid gland is producing and releasing too much of the thyroid hormones T3 and T4. This is then typically followed by a second “hypothyroid” stage during which the thyroid gland is producing and releasing too little thyroid hormone(s). This hypothyroid stage may then be followed by a final “euthyroid” stage during which normal thyroid function returns. The treatment of thyroiditis therefore depends upon the stage of the disease at the time of diagnosis. Thyroiditis in the initial “hyperthyroid” stage is treated in a similar fashion to hyperthyroidism (see “How Is Hyperthyroidism Treated” above). This may include the use of radioactive Iodine and anti-thyroid medications. Thyroiditis that has then progressed to it’s second “hypothyroid” stage is treated in a similar fashion to hypothyroidism (see “How Is Hypothyroidism Treated” above). This may include the use of synthetic forms of the T4 thyroid hormone (i.e. Levothroid or Synthroid). If the third and final “euthyroid” stage of thyroiditis occurs, then normal thyroid function has resumed and no medical or surgical treatment is required.

Thyroid pain is common with thyroiditis.
As the thyroid gland becomes enlarged during Thyroditis, this enlargement frequently causes pain. The treatment of thyroiditis therefore also may include the use of pain medications including NSAIDs. NSAIDs are particularly good at not only treating pain, but also at decreasing inflammation.
There are a number of different types of thyroid disease, so it stands to reason that there are many different things that can be done to prevent the various forms of thyroid disease that exist.Ways to prevent thyroid disease include the following: