What Is Congestive Heart Failure
Congestive Heart Failure
Congestive Heart failure, also known as “Heart Failure” or “CHF”, is a condition that occurs when the heart’s pumping power has been adversely affected. This results in the heart not be able to pump blood through the body as effectively as it should. Blood not being moved through the body as effectively as it should be means that the oxygen and the nutrients being carried by that blood do not reach the organs they are intended for as efficiently. Instead, blood that would normally be moved effectively through the heart and through the blood vessels by a healthy heart instead becomes somewhat stagnant, collecting in the heart and in the body’s blood vessels. This causes the heart, the blood vessels and the organs that the blood vessels supply to become congested with stagnant blood, hence the term “Congestive” Heart Failure.
As the heart and the blood vessels fill with stagnant blood, they stretch and stiffen. Stretching of the heart’s muscles cause the heart to become enlarged while stiffening of the heart and of the blood vessels actually serves to help move some of the stagnant blood that the heart is unable to move effectively through the heart and the blood vessels. Even though this stiffening of the body’s blood vessels helps to somewhat overcome the failing heart’s inability to move blood effectively through the heart and through the blood vessels; too much blood and fluid still collect in the blood vessels and in the organs that the blood vessels supply, causing them to become congested and engorged.
What are Risk Factors for Congestive Heart Failure?
 While a single risk factor may cause congestive heart failure, having a combination of different risk factors significantly increases a person’s risk of developing heart failure. Risk factors for heart failure include:
While a single risk factor may cause congestive heart failure, having a combination of different risk factors significantly increases a person’s risk of developing heart failure. Risk factors for heart failure include:
- Coronary Artery Disease – Coronary artery disease, also known as heart disease occurs when the blood vessels that supply the heart’s muscles with oxygen and nutrients become diseased and narrowed. The heart’s muscles, starved of adequate oxygen and nutrients become weakened. Weakened, the heart is then unable to adequately pump and to move blood throughout the body.
- High Blood Pressure – High blood pressure forces the heart to work harder as it tries to pump blood through blood vessels against the high pressure in those blood vessels. This forces the heart’s pumping muscles to work harder. Over time, this can damage these pumping muscles making them unable to properly pump blood.
- Diabetes – Diabetes increases a person’s risk of developing coronary artery disease. Coronary artery disease (see above) can damage the heart’s pumping muscles.
- Heart Attack – A Heart Attacks occurs when some of the heart’s pumping muscles die after being starved of oxygen for too long. Once dead, these pumping muscles can no longer pump blood. If a heart attack is severe enough to damage a large amount of the heart’s pumping muscles, the heart is unable to properly pump blood after this heart attack. This leads to heart failure.
What are Common Symptoms of Congestive Heart Failure?

Courtesy of the Ted Rodgers Center For Heart Research
Common symptoms associated with congestive heart failure include:
- Weakness and fatigue that results from vital organs not receiving enough oxygen.
- Shortness of breath when lying down or with activity that results from the lungs becoming congested with excess fluid.
- Wheezing or persistent cough, especially when lying down flat that also results from the lungs becoming congested with excess fluid.
- Swelling of the feet, ankles and/or legs that results from the lower extremities becoming congested with excess fluid.
- Abdominal swelling that results from the liver and the abdominal cavity becoming congested with excess fluid.
- Difficulty concentrating that results from the brain not receiving optimal oxygen from the inadequately beating heart.
- Chest pain.
- Urinating more often, especially at nighttime, as a result of the kidneys becoming congested with excess fluid.
- Palpitations that can result from an irregular or a rapid heartbeat that results from the heart trying to overcompensate for its inability to properly pump blood.
- Sudden weight gain due to fluid retention of excess fluid body wide.
- Nausea and/or lack of appetite.
- Difficulty exercising
What are the Causes of Congestive Heart Failure?
While congestive heart failure can be caused by several different things, some of the most common causes of congestive heart failure include:
- Damaged heart valves.
- Exposures to toxins like cocaine or alcohol.
- Weakening of the heart muscle resulting from heart disease, heart attack and high blood pressure.
- Infections of the heart caused by Coxsackie Virus, Human Herpes Virus 6, Parvovirus B19, Corynebacterium Diphtheriae, Staphylococcus Aureus and Borrelia Burgdorferi.
- A severe, prolonged arrhythmia (irregular heart beat).
- Congenital heart defects
- Hemochromatosis
- HIV
- Thyroid Disease
- Medications including a number of different anesthetics, certain medications used to treat heart arrhythmias, Nonsteroidal Anti-Inflammatory (NSAIDs) pain medications like Ibuprofen and Naproxen, a number of different diabetes medications including Metformin, the Thiazolidinediones and the Dipeptidyl-4 Inhibitors, some chemotherapy medications, antifungal medications and even over-the-counter decongestants.
- Excessive salt intake
- Excessive alcohol use
- Insufficient exercise
- Obesity
Why is Congestive Heart Failure Dangerous?
Congestive Heart Failure, when untreated, can lead to a number of different complications. Many of these complications result from the fact that vital organs become congested with excess fluid. This can cause them to become “water logged” and to function improperly. Additionally, because Congestive Heart Failure results in the heart being unable to provide adequate oxygen and nutrients to vital organs, this causes these congested water-logged organs to malfunction even further. As a result, Congestive Heart Failure can cause the following:
- Kidney damage, sometimes leading to the need for dialysis.
- Liver damage, because one of the liver’s primary jobs is to remove toxins from the blood, liver damage can then lead to a build-up of toxins in the blood.
- An enlarged heart.
- Damaged heart valves.
- An irregular heartbeat.
- Death, while many people with CHF will see improvement of their condition if it is properly treated, Congestive Heart Failure, when untreated can be life-threatening.
How Is Congestive Heart Failure Diagnosed?
In order to diagnose congestive heart failure, your physician initially will evaluate your medical history and perform a complete physical exam. After conducting a physical exam, if there are significant signs of Congestive Heart Failure, your physician may order one or more of the following tests:
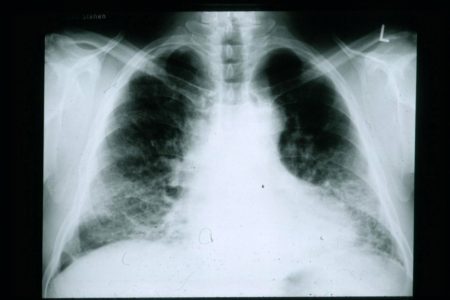 Chest X-rays – A chest X-rays allows your physician to visually assess the condition of your heart and lungs. Because people with heart failure often times have an enlarged heart and excess fluid in the lungs, a chest X-Ray can help to make a diagnosis of Congestive Heart Failure.
Chest X-rays – A chest X-rays allows your physician to visually assess the condition of your heart and lungs. Because people with heart failure often times have an enlarged heart and excess fluid in the lungs, a chest X-Ray can help to make a diagnosis of Congestive Heart Failure.- Blood Test to Assess Liver and/or Kidney Function – Because heart failure frequently affects the liver and the kidneys, blood tests can be done to determine whether or not the kidneys and/or liver are functioning properly. An improperly functioning liver and/or kidneys maybe evidence of heart failure.
- Blood Tests to Assess BNP Levels – BNP, or “Beta-type Natriuretic Peptide is a protein that heart muscle creates in response to being stretched. The more stretched heart muscle becomes, the more BNP it makes. Because heart failure causes stretching of heart muscles and enlargement of the heart, BNP levels will be elevated in a person with heart failure.
- Echocardiogram – An echocardiogram is an ultrasound of the heart. Heart failure results when the heart muscles are not contracting properly, and the heart is not beating forcefully enough. Ultrasound of the heart allows your Doctor to assess how well the heart’s muscles are contracting.
- Electrocardiogram (EKG)– A EKG allows your Doctor to assess your heart rhythm. Frequently, people with heart failure have abnormal heart rhythms.
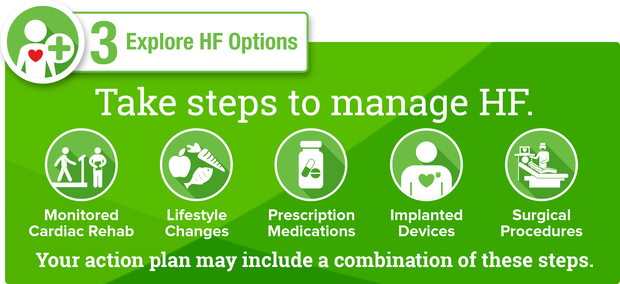
How is Congestive Heart Failure Treated?
Frequently, Congestive Heart Failure is treated using one or more medications combined with lifestyle modifications and cardiac rehabilitation. In some cases, especially when lifestyle modifications, cardia rehab and medications aren’t effective, surgical procedures may also be used to treat CHF.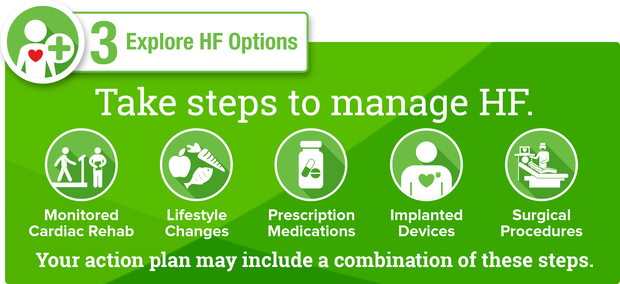
Lifestyle modifications used to treat Congestive Heart Failure include:
- Eating a low-salt diet (i.e. no more than 1500-2300mg of sodium per day).
- Exercising regularly, this means getting at least 150 minutes of moderate aerobic activity every week, 75 minutes of vigorous aerobic activity every week or a combination of the two.
- Smoking cessation
- Weight loss and/or maintaining a healthy weight with a BMI that ideally lies between 18.5-24.9.
- Tracking and limiting fluid intake. Because people with heart failure retain too much water, they should limit the amount of water that they ingest each day. While healthy people are encouraged to drink at least 8 cups of water a day, people with CHF should limit their total fluid in-take to 4 cups of liquid a day.
- Avoiding alcohol
- Avoiding caffeine
Medications used to treat heart failure include:
- Beta Blockers – Beta Blockers are medications that can both reduce high blood pressure and correct abnormal heart rhythms. High blood pressure and abnormal heart rhythms can both causes and result from heart failure, so treating them with Beta Blockers can be beneficial.
- ACE Inhibitors – ACE inhibitors are medications that can widen blood vessels. Widening blood vessels can improve the flow of blood within blood vessels, making it easier for the heart to pump blood through them.
- Diuretics – Diuretics are medications that help the body to eliminate fluid. Because heart failure is characterized by the excessive buildup of fluid throughout the body, diuretics can prove very helpful in treating CHF.
- Angiotensin II Receptor Blockers – Angiotensin II Receptor Blockers work in much the same way as ACE inhibitors, widening blood vessels and improving the flow of blood through them.
- Inotropes – Inotropes are intravenous medications that are used to individuals who are hospitalized with severe heart failure.
- Aldosterone Antagonists – Aldosterone Antagonists work like diuretics, helping the body to rid itself of excess fluid. Unlike many diuretics, Aldosterone Antagonists do not affect levels of Potassium in the blood. This means that, in addition to helping rid the body of excess fluid, they also can help the heart to contract more strongly.
- Digoxin – Sometimes also called Digitalis, Digoxin is a medication that causes failing heart muscles to contract more strongly.
Cardiac Rehabilitation
Cardiac rehabilitation programs are designed to improve the heart health of people suffering from congestive heart failure. They involve exercise counseling and training, counseling aimed at teaching patients stress reduction techniques and heart healthy living education.
- Exercise Counseling and Training involves teaching people with CHF how to exercise in a manner that is both safe and that promotes improved heart health.
- Stress Reduction Counseling involves helping patients with CHF learn how to better identify and combat everyday sources of stress in their lives. Stress can place an unnecessary strain on the heart, and learn to combat it can therefore improve heart health.
- Heart Healthy Living Education involves teaching patients with CHF how to identify and manage risk factors for poor heart health. It also involves teaching heart healthy eating habits and heart healthy lifestyle modifications like alcohol avoidance and smoking cessation.
Surgical procedures used to treat heart failure include: 
- Coronary Artery Bypass – CHF often results when heart muscle being supplied by narrowed or disease blood vessels becomes damaged from a lack of adequate oxygen. Coronary Artery Bypass involves removing diseased blood vessels from the heart and replacing them with healthy ones that can better supply oxygen and nutrients to heart muscle.
- Heart Valve Repair/Replacement – Heart failure sometimes results from a faulty or damaged heart valve. When this is the case, the valve will frequently be repaired or replaced.
- Placement of an Implantable Cardioverter/Defibrillator (ICD’s) – ICD’s are implantable devices that can detect the heart’s rhythm. Because people with heart failure often have abnormal heart rhythms, when these devices detect an abnormal rhythm, they give the heart an electrical shock to correct it.
- Cardiac Resynchronization Therapy (CRT)/Biventricular Pacing – Involves placing an implantable device that, like an ICD can send electrical impulses to the heart to regulate it’s rhythm and the strength with which the heart’s muscles contract.
- Placement of a Heart Pump – Heart pumps are devices that are placed in either the abdomens or the chests of people with heart failure. They are attached to the weakened heart, and they help it to contract more effectively.
- Heart Transplant – When heart failure does not respond to lifestyle changes, medications of more conservative surgical management, the failing heart may then be replaced with a healthy, transplanted heart.
Be sure to check out our website www.TheTwinDoctors.com and please connect with us on all of our social media outlets at TheTwinDoctors.
 May 19, 2018
May 19, 2018
 While a single risk factor may cause congestive heart failure, having a combination of different risk factors significantly increases a person’s risk of developing heart failure. Risk factors for heart failure include:
While a single risk factor may cause congestive heart failure, having a combination of different risk factors significantly increases a person’s risk of developing heart failure. Risk factors for heart failure include:
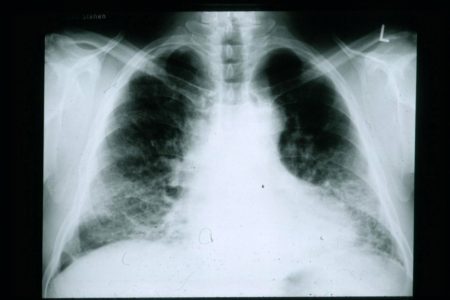 Chest X-rays – A chest X-rays allows your physician to visually assess the condition of your heart and lungs. Because people with heart failure often times have an enlarged heart and excess fluid in the lungs, a chest X-Ray can help to make a diagnosis of Congestive Heart Failure.
Chest X-rays – A chest X-rays allows your physician to visually assess the condition of your heart and lungs. Because people with heart failure often times have an enlarged heart and excess fluid in the lungs, a chest X-Ray can help to make a diagnosis of Congestive Heart Failure.