5 things that can go wrong with your IUD and what to do about it.
 May 19, 2018
May 19, 2018
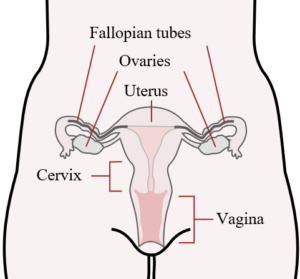
Female Reproductive Tract
Many different strains of Streptococcus (a.k.a Strep) and Staphylococcus (a.k.a Staph) bacteria can normally be found either in or on the human body. These bacteria are said to be “colonizers” of the human body, and their presence either in or on the body is not considered to be abnormal or unhealthy. Group B Beta Strep, commonly referred to as GBS, is one of these common human colonizers. As such, GBS is typically found in the digestive and/or reproductive tracts of approximately 25% of people.
Because 25% of women carry the GBS bacteria either in or around their vaginas, there is a risk that newborn babies can be exposed to the bacteria during delivery. While the GBS bacteria can be found normally in or on the adult human body, and it’s presence there is neither abnormal nor unhealthy, exposure to it as a newborn baby can cause serious illness. For this reason, steps are taken during pregnancy to limit the exposure of newborn babies to the GBS bacteria if their Mothers are among the 25% of adult women who carry it either in or around the vagina.

GBS Swab Kit
To prevent newborn exposure to GBS, all pregnant women receiving routine prenatal care typically have vaginal and rectal cultures done to test for the GBS bacteria. These cultures are normally done around the 36th week of pregnancy. When GBS cultures are done, it simply involves having one Q-Tip placed in the vagina and another Q-Tip placed on the anus.
The primary concerns surrounding GBS and pregnancy are those involving newborn infants being exposed to the bacteria during delivery. However, there is also evidence that women who carry the GBS bacteria in or around their vaginas may be at a slightly increased risk for preterm labor, their bags of water breaking earlier than normal and for infections of the uterus and/or placenta. The risks for all of these GBS related pregnancy complications are however thought to be extremely negligible. So much so in fact that pregnant women are not even routinely tested for GBS at the outset of their pregnancies. Nor are they routinely treated for vaginal or rectal GBS at the outset of their pregnancies if either is detected.

Vaginal/Rectal Cultures are done between the 35th and 36th week of pregnancy to test for GBS.
When reaching the 36th week of pregnancy, all pregnant women should be tested to see if they are among the 25% of women who carry the GBS bacteria in or around the vagina. If women test positive for the GBS bacteria at the 36th week of pregnancy, they should be given intravenous (IV) antibiotics when they present to the hospital in labor. Administration of IV antibiotics while in labor should eradicate the GBS bacteria before most babies can be exposed to it during delivery. If IV antibiotics are not given to GBS positive women before delivery, approximately 1 in 200 babies exposed to the GBS bacteria will get sick from it.
While any newborn baby exposed to the GBS bacteria can get sick from it, there are certain babies that are more likely to get sick when exposed. These babies include those born prematurely, those born to women who had a fever during labor, those born to women who have previously had newborn babies with GBS infections and those born to women whose bag of water was broken for more than 18 hours before delivery. When newborn babies do get sick as a result of being exposed to the GBS bacteria, a number of complications can result. These complications include pneumonia, meningitis and bacteremia.

Pregnant Woman Getting IV Antibiotics in Labor
The vast majority of newborn babies that are exposed to the GBS bacteria are exposed during delivery. Therefore, all women who test positive for having the GBS bacteria in or around the vagina are treated with IV antibiotics while in labor. This helps to largely eradicate GBS from in and around the vagina before delivery. When women with the GBS bacteria in and around the vagina are treated with IV antibiotics before delivery, the likelihood that their newborn infant will get sick from GBS drops dramatically. Falling from a 0.5% to chance to a 0.00025% chance.

Sick Newborn Baby
Newborn babies with GBS infections are primarily treated with IV antibiotics. Additional supportive care like the administration of IV fluids and even the use of mechanical ventilation (i.e. a breathing machine) may also be used depending upon how severe the baby’s illness is.